Researchers have been mining faecal bacteria (shown here in a coloured electron microscopy image) for those that might help to boost cancer therapies.Credit: Steve Gschmeissner/Science Photo Library
A potent bacterium in the human gut can supercharge the effects of some cancer drugs in mice — and researchers are now planning a clinical trial to test whether it could do the same in people. The microbe stimulates cells in the immune system called dendritic cells, which go on to amplify the effects of cancer drugs that unleash the body’s own defences against tumours.
The work, published on 14 July in Nature1, is the latest in a wave of increasingly sophisticated studies that are unpicking the relationship between microbes in the body and responses to cancer treatment, says Marlies Meisel, who studies immunology and microbiology at the University of Pittsburgh in Pennsylvania and was not involved in the study. “This is a really valuable reservoir of bacteria,” she says. “These researchers have leveraged a gold mine.”
‘A huge effort’
Until now, the humble bacterium Hominenteromicrobium mulieris had received little acclaim. Discovered only three years ago, it thrives quietly in the low-oxygen, nutrient-rich environment of the human intestine. Hiroyoshi Nishikawa, an immunologist at the National Cancer Center in Tokyo, and his colleagues came across a new strain of the microbe while analysing faecal samples from 50 people with cancer who had been treated with drugs called immune checkpoint inhibitors.
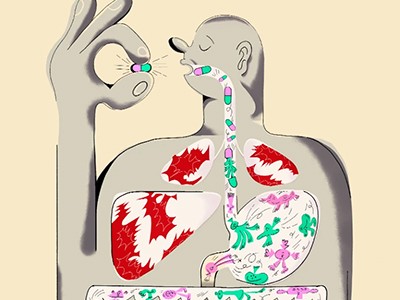
How gut bacteria could boost cancer treatments
These therapies can have remarkable effects, sometimes empowering the immune system to drive advanced cancers into long-lasting remission. But they do so in only a fraction of the people who receive them, and researchers have been searching for a way to broaden the drugs’ reach.
To learn more about why some people respond to checkpoint inhibitors and others do not, Nishikawa’s team used the faecal samples they had collected from people with cancer and transplanted them into mice with tumours. Mice that received transplants from people who responded well to the checkpoint inhibitor benefited more from this therapy than did mice with transplants from people who did not respond to the drug.
Nishikawa decided — naively, he now says — to track down the microorganism in the faecal transplant that was responsible for the difference. It would take his team about a year and a half to pinpoint the microbe that had the biggest effect: a strain of H. mulieris. “I’m an immunologist, not a microbiologist,” he says. “I didn’t know it would take such a huge effort.”
With that information in hand, the team was able to sort out how H. mulieris improved responses to checkpoint inhibitors. In mice, the microbe stimulates dendritic cells, which can travel through the blood to tumours. There, the dendritic cells activate a subset of other immune cells, called T cells, that can recognize and destroy cancer cells. This heightens the effects of checkpoint inhibitors, which work by unleashing those same tumour-targeting T cells.